Proposed Changes to Clinical Training in Occlusion
I’m hoping to discover what it is that people really want to learn and what their aim is when they include our occlusion courses as part of their personal development portfolio.
We have a problem at the moment that I think relates to the fact that, despite some recent updates, SDS have been running what is essentially a 30 year old course, teaching basically the same stuff in the same way for almost all that time. People do seem to enjoy the 2-day POISE introductory course and find it to be a valuable source of new information and skills, but they say they will sign up to attend the next level courses (over 90%) and then when it comes to booking on the next phase it just doesn’t happen – so we have had to cancel every single one of the POS equilibration courses for the last two years in all locations. This is despite fantastic feedback from the earlier POS courses and some very keen dentists who still keep in touch and send me cases to treatment plan, etc. A re-think is definitely needed and the course must change in order to appeal to today’s dentists.
The redesign I am considering is to shift the focus of the course away from pain and headaches to helping dentists solve the problem of how to rebuild the appearance and function of damaged dentitions, whether it be through wear, caries, extraction or whatever combination you care to imagine. Obviously we will still have to look at TMJ health and muscle pain as part of this, it just won’t be the main focus any more.

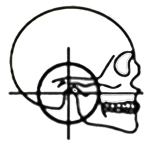
Want to know how to turn this ...
We used to run introductory 2-day courses, usually at weekends. My idea now is to run 2 x 1-day courses approx a month apart, keep the numbers down to 10-12 delegates and using 5 or 6 surgeries so that everyone can do the clinical stuff in pairs in a more realistic clinical environment so they get a more positive learning experience. The first day would include impression taking, facebow records, centric relation records and anterior deprogrammer construction, fit and adjustment, in addition to all the necessary theory. On the second day, a month later, the delegates would fit lab made stabilisation appliances from their records they had made on the first day, along with more advanced theory stuff and use of articulators by re-mounting the lower cast with a new CR record (after using the anterior deprogrammer for a month) and cast equilibration.
The next stage in this first year course would run in a similar way over 8 more days, a month apart again, but would involve bringing real patients along to be co-diagnosed by the group and treated, first with appliances, then equilibration and/or restoring using reversible means (e.g. direct composites, dentures, long-term appliances, etc.).

... into this, using acrylic and composite?
The following year’s course would move onto permanent restorative/prosthodontic methods, with more patients being treated, staring with anteriors, then, a posterior quadrant, then a full mouth (as currently occurs on the IRS and ARS courses).
There would also be online teaching, reading and practical tasks/projects that would need to be studied between all sessions.
I am in discussions about making the resulting 2 year course a major part of a diploma/MSc course accredited by a UK university (3 or 4 possibilities being considered).
What do you think? Feedback needed fairly urgently please 🙂
Regards, Andy Lane

Andy-I like it!
I think that on the front end I would like to see more than one day. This will help with group cohesion and also to explore concepts rather than just ‘get through’ the exercise.
Keep me posted-sounds great!
Hi Miguel, I wanted to make it easier for people to attend and a one day course is much better I think, but a possibility would be to start in a hotel Friday lunchtime, spend the afternoon on lectures and have a meal together before the full day with the clinical/hands-on sessions on Saturday – how does that sound?
Andy,
Love the idea and the more practical integration into treatment planning, but also was keenly waiting for you to announce the next POISE course dates because there is very little else around which specifically tackles TMJ health, facial pain and splint therapy.
Perhaps the missing link between your intro course and equilibration and more detailed concepts IS precisely this integration you’re thinking of.
Hope that comes across constructively.
Best regards,
Sahir
Thanks Sahir. I don’t really want to lose the TMJ element completely, but this might not seem relevant to so many dentists at present, compared to, say, treating the worn or collapsed dentition.
The problem with the current POISE course is that it’s a huge amount of work in a short space of time, but if we reduced the length of time spent making an appliance in the lab and spent more time on the clinical work it might make more sense and give people something really practical they could take back into practice the following Monday morning.
I’d also really like to get Mike Melkers, who replied above and runs the “Nut and Bolts of Occlusion” courses in the USA, involved in the main part of the course, which would give it a great international perspective, especially on patient motivation and treatment planning.
Cheers, Andy
Maybe I am unusual but the bits I am interested in is the TMJ pain and the occlusal equilibrium. I personally have 2 difficulties with the full mouth rehabilitation in that a) I have spent a lot of time and money doing other courses for this and more crucially b) I just don’t have enough patients willing to invest in their teeth to undergo extensive treatment options. Maybe it’s my sales technique? Best of luck with it all.
Thanks Samantha.
I’m afraid treating TMJ pain isn’t high on many dentists’ wish lists at present, maybe because it’s hard work, more of an art than a science and poorly rewarded.
Mike and I are planning to run a course together on the “sales techniques” as you put it 🙂 – he’s great on the communication side and can help us all to convert more patients to take advantage of the long-term benefits we can offer them.
Andy-that would be a pleasure. Seriously…the reputation and history of POISE-it would be an honor!
To the questions…
1-I think group cohesion is key; not only for commonality and learning but to build autonomous study support groups for after and between courses. We have done the N&B courses all over the world and one thing is VERY consistent. Those that keep in touch implement and thrive. Not just by achieving success but more so by pushing past challenges.
2-Which is a PERFECT segue into Samantha’s comment and concern. We learn but can we implement. This is a HUGE point-if we cannot implement and incorporate our knowledge to better serve our patients and be compensated for it, CE become entertainment, frustration or both.
I think it is important-in my journey and experience…and frustration-that we not strive for ‘full mouth rehabilitation’ but rather meeting our patients’ goals. Understanding them, listening…and then offering solutions “Based on your goals, as I understand them-what I recommend is__________.” Try using that phrase for the next 30 days. It will change things. It will lead to single crowns…it will lead to more ‘full cases’, and the patient will lead us.
“Patients carry their own doctor inside. They come to us not knowing that truth. We are at our best when we give the physician who resides within each patient a chance to go to work.” Dr. Albert Schweitzer
LOL-sorry…went off on a tangent! Now back to our regularly scheduled program!
I am not quite sure about the new format Andy because there are so many courses on the market which offer to teach full mouth rehabs. What I liked about the SDS was it took you back to the very basics in occlusion . I would like a bit more emphasis on the TMJ . I quite like Mike’s idea of having study support groups to run simultaneously.
Thanks for your feedback Aparna. I’m not sure there are so many courses that teach with clinical work on dentists’ own patients, but happy to be corrected. That’s always been the strength of our courses I think; the proper clinical hands-on stuff like equilibration and appliance delivery. The study-club approach is definitely what we should be aiming at because everyone learns so much from interacting and discussing problems with people who are going through the learning same process.
I would certainly like to bring in more TMJ teaching if there is the demand, which hopefully will materialise eventually 🙂
You must let me know how all your lovely patients that we co-diagnosed/treated are getting along!
Cheers, Andy
Hi Andy
I would certainly agree with your comment: “The problem with the current POISE course is that it’s a huge amount of work in a short space of time, but if we reduced the length of time spent making an appliance in the lab and spent more time on the clinical work it might make more sense and give people something really practical they could take back into practice the following Monday morning.”
However, what attracted me to the course you and Roy were running was the fact that the basics were taught first, in a distance learning format and I felt that would be crucial to my own understanding of the problems that would be encountered every day, from a single restoration to a full mouth rehab. I still believe that now and utilise the knowledge I gained on a daily basis.
I can certainly understand the difficulties you face in achieving the correct balance to attract delegates who can see an advantage in their every day practice and yet are also willing to learn the theory required to apply the practical skills effectively and safely. What you have described could well achieve that goal and certainly appeals to me.
With regard to a diploma / MSc – what would be the additional requirements for potential candidates to fulfil?
Kind regards
Colin
I had the privilege of completing combined poise / poise 2 courses 2010 – 2011 and feel that GDPs are not progressing from one to the other because a lack of interest in TMD but a lack of free time. The only negative comment I heard from others on the course was that each stage took up a whole weekend. Those who work Monday to Friday could find it hard to commit to both Saturday and Sunday also.
The lack of undergraduate teaching in the subject means that the missing core of occlusion / anatomy knowledge necessary may have to be given as ‘distance learning’ prior to the first day.
Andy I think you are definitely on the right track with the proposed changes.
Thanks very much Mark – so do you think Saturday courses once a month would be a better format?
Whilst I understand the reasons for including making our own Stabilisation Splints (it helps us to understand the 3 dimensional relationships better) maybe we’re doing it too early and it would be more rewarding and encouraging to learn how to adjust and fit a lab-made appliance – after all, that’s a really hard thing to get right anyway, without having to do the lab-work!
I do have the distance learning modules ready to go, but we have found some resistance to completing them properly sadly; most of the exercises I ask them to do don’t get done, which is frustrating – maybe I need to re-think these?
Hi Andy
I enjoyed the POS course when I completed it 2 years ago. I don’t see why there would be a good reason for there being resistance to completing the distance learning modules as I didn’t think there was much to them. The only thing that I remember thinking at the time of doing them, was that I wasn’t always sure how the results of the exercises (e.g. number and type of contact points, mandibular movement measurements, questionnaires) would have actually effect patient management.
The actual weekend was long but enjoyable, I was happy playing in the lab making a splint as it helped me visualise what we were attempting to achieve with the splint. But more time on clinical work to give people that practical skill on their first day back at work would be no bad thing! The first splint I fitted took me a long time… 🙂
I was really interested in doing the POS equilibration course afterwards, but lack of interest from patients to travel from mid-Wales made me decide otherwise.
The proposed course plan sounds a good one. Shifting the focus from pain and headaches to more restorative based occlusal applications may attract more interest from more restorative minded dentists who may dismiss the former course as it’s of no interest to them. I’ll make a guess and say there’s more dentists interested in restorative work (and ignoring the thought of TMJs and pain). Cardiff University do distance learning modules of 5 units each year. Several years ago I applied to do the TMJD module with R Jagger. Just needed, I think, 6 dentists to pay a £25 course fee…the module was shelved as there wasn’t enough interest. Which I thought was shocking considering Cardiff send the application forms to all dentists in Wales. I think anything related to the TMJ and pain puts people off as they have little understanding of the subject and it all comes across as a Dark Art that they’d rather not delve into, but masked under a more restorative guise the courses may attract more people…?
Hi Andy,
That sounds very good.
Unfortunatly, occlusion and TMJ have not been been given enogh time at the undergraduate level, and it was always a ” very boring subject ” for us to digest and understand. I have attended the full year couse and I have to admit that your type and style of teaching was unique which finaly I did understand the occlusion and TMD.
I am currently doing MSc in aesthetic and restorative dentistry and your course has helped me a lot and saved me time. During one of our hands-on resedential, I have seen a lot of dentist (some of them were older than me) were having difficulties in muscle palpation and identifing the CR position.
I think doing some changes as you and athers mentioned will be very helpful. however, I think the old style of teaching was unique.
Good luck and I will be always available if you need any help.
Helmi
Dear Dr. Andy,l am a female in my 60’s. For 8.5 years l have this excruciating pain located only in my upper gums. l took amtriptilin, gabapentine,tramadol etc. etc. and nothing did help, now l am taking carbazepine(tegretol) 2 pills of 15.5 per day, plus mirtazepine for insomnia and lost of appetite and depresion caused by the horrific pain.
I just had an MRI that didn’t show a culprit either,The trigeminal nerve he sais is ok.
My question is: is it possible that a 35 year old 12 piece metal bridge on my upper gums be the cause of this 8.5 years awfully burning pain? l just had an MRI and Dr say that nothing wrong showed up
I went to dentists, periodontist, oral surgeons, mandibular CT scans etc. and no one suggest that my old bridge may be the culprit of my excruciating pain.The XR do not show sinus problems, infections, absess.Apparently dentists do not see this old metal bridge be the cause of this terrific gums burning pain.
Dr Just incresed the dosis of the medicines but the gum pain still umberable and l am a zomby. Dr Andy,Is it possible that the extensive old metal bridge agravated the ramifications of the trigeminal nerves on the upper gums to the point of damaging the nerves? Is that suppose to show in the MRI(contrast and no contrast) Nobody offer a possible solution and l cannot stand any more. Should l take all my upper teeth out and wear dentures?Please help!!!!!!!!!!
Hi Monique, I’m sorry to hear about your troubles, it sounds awful. May I ask where you are based? I have some theories about why people get these symptoms but nothing shows on MRI or radiographs. If you prefer please email me on andylanebds@gmail.com
With warm regards, Andy